Studies show that older adults taking antibiotics regularly are at increased risk of ulcerative colitis and Crohn’s disease, particularly those for intestinal infections. The highest risk occurs two to two years post-antibiotic usage.
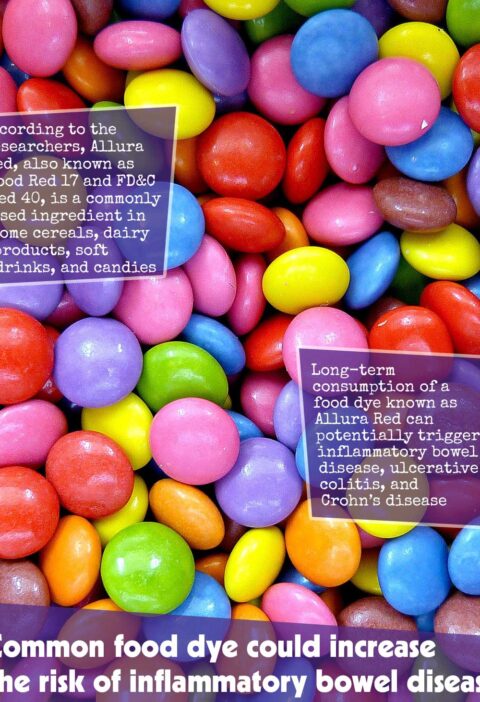
Environmental factors could be the source of Inflammatory Bowel Disease. At present, over 7 million people worldwide are living with this condition and researchers anticipate its prevalence to continue growing over the coming decade.
Whilst antibiotic use’s influence on risk for inflammatory bowel disease among younger individuals has been widely recognized, its exact association between use of antibiotics and risk for all age groups remains uncertain. Therefore, further investigation must be conducted in order to ascertain an accurate association between antibiotic use and risk for all age groups.
For further insight, the research team utilized medical records of people aged 10 or above with no history of inflammatory bowel disease.
Researchers sought to explore whether timing and dosage of antibiotics could influence the development of inflammatory bowel disease; as well as whether their influence varied depending on type or antibiotic treatment regimen used.
This study included over 6 Million individuals, approximately 50% being females, who received one or more antibiotic courses between 2000 and 2018. Of this group, 91% received at least one course between 2000 and 2018.
Over this period, approximately 36,017 were diagnosed with ulcerative colitis and 16,881 people with Crohn’s disease.
Results indicated that antibiotic use can increase the risk of inflammatory bowel disease regardless of age; however, an elevated risk was seen among older individuals.
According to the results, people aged 10-40 had a 28% greater risk of being diagnosed with inflammatory bowel disease, while those between 40-60 were 48% more likely and those over 60 47%.
Crohn’s Disease had a slightly increased risk compared to Ulcerative Colitis: it rose 40% for individuals between 10-40, 62% between 40-60, and 51% among those over 60 years of age.
Each time I took an additional course, the increased risk was cumulatively increased – 11% higher for every additional course taken, 15% higher, 14% higher respectively.
People taking five or more antibiotics at once are at greatest risk, with 69% greater risks among 10-40 year-olds, double that risk among 40-60 year-olds, and 95% increased risks among those aged 60 years old and beyond.
Studies revealed that antibiotic use at specific times could increase risk for inflammatory bowel disease, specifically two to three years post-medication use and gradually decreasing from there.
Individuals aged 10-40 were more prone to developing inflammatory bowel disease within two to four years of taking antibiotics; this risk declined to 13% after four to five years of therapy. By comparison, 66% opposed 21% among individuals between 40-60 years of age while for individuals over 60 it stood at 63% as opposed 22%.
Fluoroquinolones and nitroimidazoles antibiotics commonly prescribed to treat gut infections pose the highest risk for inflammatory bowel disease. Because broad spectrum antibiotics aim to eliminate many different microorganisms that might cause illness, not just those responsible for illness.
Nitrofurantoin was the only antibiotic type not linked with an increased risk of inflammatory bowel disease; narrow spectrum penicillins had some influence but at lower levels.
Research supports other findings which demonstrate how gut microbiota play an essential role in health and well-being, with certain antibiotics having significant impacts on this microbial community, potentially altering its structure.
This study is observational in nature and cannot establish cause and effect. Additionally, according to the research team’s account there is no data regarding which medications were taken by participants or in what quantities.
Researchers suggest there could be biological reasons for their results, including weakening and reduction of gut microorganisms due to age – likely worsened by antibiotics use.
Antibiotic use may wreak further havoc with an individual’s intestinal microbiota and hinder its recovery process.